Inhaling Immunity: UNC Research on Inhalable COVID Vaccines
The University of North Carolina has presented its data in Nature Biomedical Engineering regarding the creation and efficacy of an inhalable vaccine for the SARS-CoV-2 virus. The big players of COVID vaccines (Pfizer, J&J, etc.) have all put out vaccines that require both a cold chain and a syringe in order to get to the patient. This requirement of a cold chain is responsible for a lot of the issues of accessibility that took place during the height of the pandemic and strained global logistics to a significant degree. Besides this, inhalable vaccines deal with needle phobia and more directly expose vulnerable respiratory tissues to the vaccine when compared to intramuscular injections.
While the technology had some presence before the pandemic, COVID-19 has presented a silver lining by bringing inhalable vaccines more into the spotlight. This has reinvigorated researchers who were trying to develop a better way to respond to tuberculosis in the form of a vaccine and could do a lot to prevent respiratory infections.
Exosomes as a Better Vaccine Vector
The vaccine takes advantage of nanoparticles and their ability to bind proteins to their surface. The protein in question is the receptor binding domain (RBD) of the SARS-CoV-2 virus. The RBD is the section of the SARS-CoV-2 viral protein responsible for binding to the receptors on human epithelial cells e.g., in the lungs. This combination creates a particle that interacts with host cells initially in the way the virus would but does not have the necessary viral instructions to infect the host.
The research described in the University of North Carolina article mentions the use of liposomes (artificial vesicles made from a lipid bilayer) in previous vaccines like Pfizer’s and Bio-N-Tech’s injectable COVID vaccines. These vaccines are able to use liposomes with attached viral RNA to introduce the patient’s immune system to viral proteins safely in order to train the immune response.
In this research article, the team makes use of this same concept of the RBD binding to a particle as a means of inducing immunity but changes out the liposome for an exosome, a membrane-bound 40-150nm extracellular vesicle. They produced these exosomes using lung spheroid cells (LSCs) with the theory in mind that these native nanoparticles (NPs) would be better absorbed and accepted by the patient’s immune system. The researchers believed it could be better at being a vaccine vector than the liposomes used in other projects.
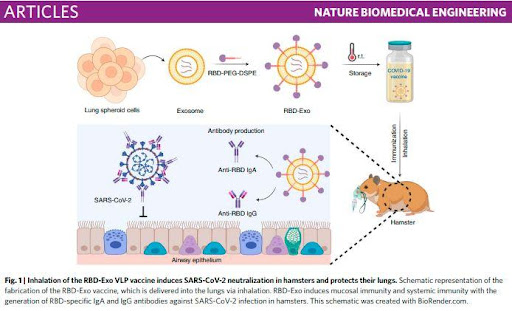
This formulation of the vaccine has the added advantage of being able to break the storage constraints of injectable vaccines. Rather than requiring refrigeration and thus a cold chain for transportation this vaccine is able to be stored and transported at room temperature and maintain the majority of its efficacy.
Nebulized Exosome-based Vaccine OutPerforms All Others in Rodent Model
The experiments in this article involved exposing rodent test organisms to vaccines and examining their body fluids post-exposure. These vaccines varied depending on whether their vector was an exosome or a liposome and whether they were administered by injection or inhalation. These experiments thankfully came with conclusive data that gives cause for hope about inhalable vaccine research for SARS-CoV-2.
Exosomes were correlated with increased interaction with the cells of the lung tissue in both injected and nebulized vaccines with nebulized vaccines having increased interaction in both cases. These results are in keeping with the previously measured load efficiencies (ratio of protein mass to that of the particle they are attached to) of exosomes vs. liposomes. These load efficiencies were calculated to be 2.08% in exosomes, and 0.41% in liposomes; thus, they are able to deliver more viral protein per dose of vaccine. This increased ability to carry viral protein stacks on top of the benefit of delivering a vaccine directly to the cells most vulnerable to an illness. Exposing respiratory cells to the vaccine directly shows a marked advantage due to there being less time and space for the antigens to dissipate.
The need to quickly and easily vaccinate populations will go up as SARS-CoV-2 continues to mutate. Already many countries are faced with the problems of a lack of ability to distribute vaccines to their populations due to the need for a cold chain and unwillingness due to needle fear. Considering that approximately 20% of adults are estimated to have a needle phobia inhalable vaccine could help grab the low-hanging fruit of public health participation.
Any developments that can increase vaccination rates contribute toward the world being able to move forward from the pandemic and treat diseases that previously weren’t fought as well. Being able to produce inhalable vaccines will make prevention and treatment for future SARS, MERS, and other respiratory infections much more effective. Research like this into more stable, easy to transport, and easy to administer vaccines is a critical component in the infrastructure of life-saving.
©www.geneonline.com All rights reserved. Collaborate with us: service@geneonlineasia.com








