Novel Bioengineered Wearable Edgeless Skin Brings Hope to Revolutionize Plastic and Reconstructive Surgery
Researchers at Columbia University have devised a way to grow bioengineered skin in complex, three-dimensional shapes, making it possible to use skin cells to construct seamless “biological clothing” that can be transplanted directly onto damaged body parts. The research team reported their findings in a paper published in the January 27 issue of the journal Science Advances.
Related articles: 3D Printing Creates Tactile Artificial Fingers Resembled to Real Human Fingers
Challenging the Prevailing Paradigm in Skin Bioengineering
Tissue engineered skin has been under development since the early 1980s. Nowadays, engineered skin grafts used for transplantation are prepared in flat sheets with open edges. When it comes to anatomically complex body sites such as hand and face, conventional skin grafts cannot cover these parts effectively and have to be stitched together around irregularly shaped body parts, making the transplantation process arduous and time-consuming and worsening the aesthetic and functional outcomes.
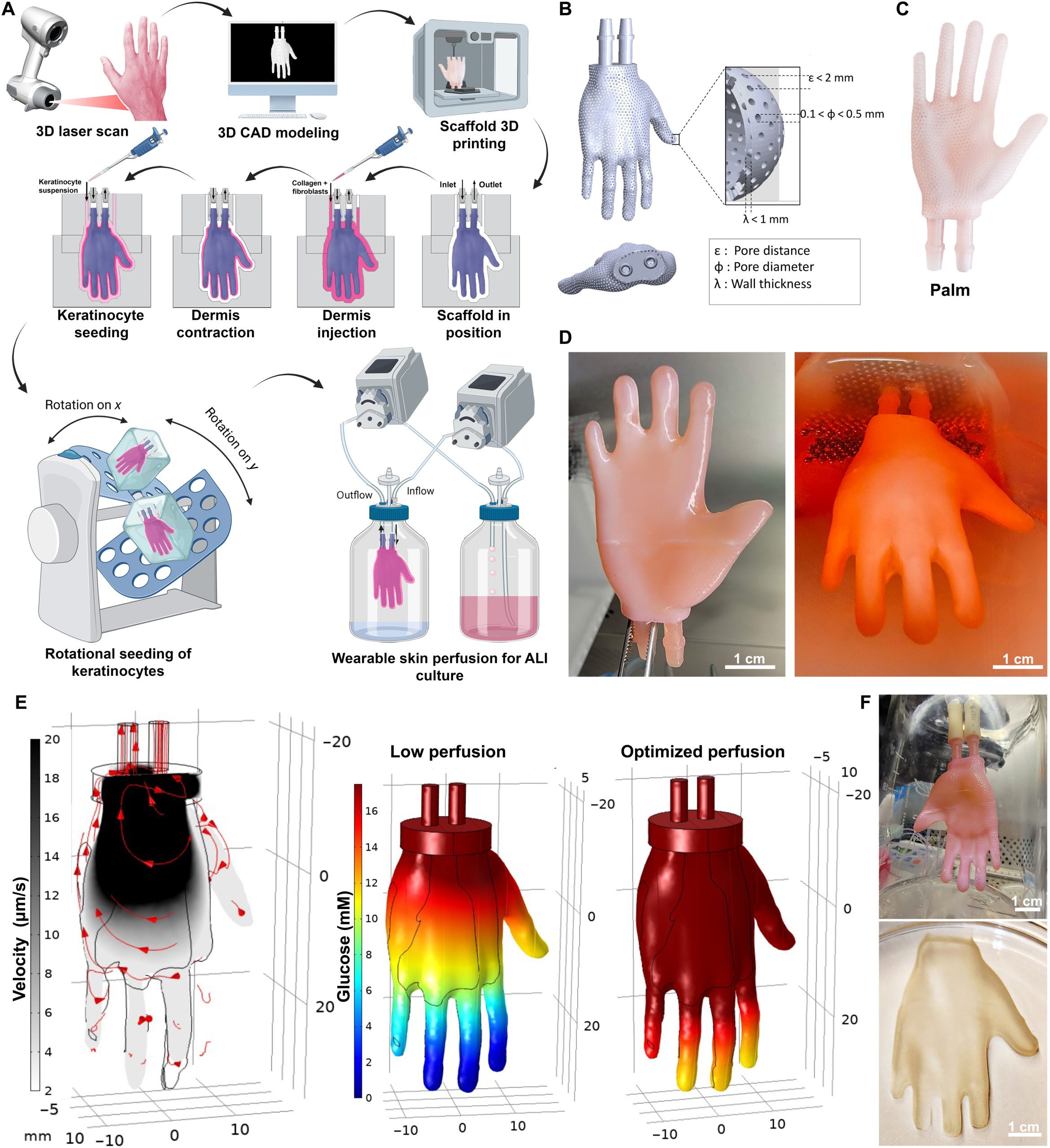
A team of researchers and bioengineers led by Dr. Hasan Erbil Abaci from the Columbia University Irving Medical Center has successfully engineered and grown wearable edgeless skin constructs (WESCs). The process of creating the novel skin grafts begins with a 3D laser scan of the target structure, such as a human hand. Next, a hollow, permeable model of the body part is crafted using computer-aided design and 3D printing. The exterior of the model is then seeded with skin fibroblasts, which generate connective tissues and collagen needed to give the skin its structure. Lastly, the surface of the mold is coated with keratinocytes (cells that constitute most of the epidermis), while the interior is perfused with growth media, which support and nourish the graft as it develops.
The skin is removed from the model in one three-dimensional piece once the cells have grown into actual skin, positioned around the actual body part for which it was made, and sutured in place. The researchers also made flat pieces of bioengineered skin with the same procedures they used to make the 3D scaffold, both processes taking about 3 weeks.
Testing the Novel Bioengineered Skin Constructs in Mice
To test out this innovative 3D engineered skin, the team designed a mouse hindlimb scaffold and then used it to generate a mouse version of the WESC composed of human skin cells. Vascularized WESC was then removed from the scaffold as a single piece and implanted onto the left hindlimb of nude mice with the skin covering the part for transplantation removed. After that, WESC was placed seamlessly like a piece of clothing that fit specifically for the wound. “It was like putting a pair of shorts on the mice,” Dr. Abaci recalled.
The whole surgical process only took about 10 minutes. 4 weeks later, the graft was completely integrated with the surrounding mouse skin, and the mouse reacquired the full functionality of the lower limb. In addition, the current study of Dr. Abaci’s team also revealed that the continuous 3D skin grafts demonstrated better mechanical and functional properties than conventional, pieced-together grafts.
The Hope for Customized “Biological Clothing” for Transplantation
Given the fact that mouse skin heals differently than human skin, the researchers plan to test the novel 3D skin grafts on larger animals with skin biology that more closely matches that of humans following the remarkable success of mouse experiments. It is anticipated that clinical trials in humans may take place several years later.
In the future, Dr. Abaci believes that it could be possible to create personalized grafts from a patient’s own skin cells. For example, a seamless “glove” of skin cells that can be easily slipped onto a severely burned hand. This would minimize the need for suturing, reduce the length of surgeries, and improve aesthetic outcomes. There is also the potential for this technology to be used in face transplants, probably bringing hope to revolutionize plastic and reconstructive surgery.
©www.geneonline.com All rights reserved. Collaborate with us: service@geneonlineasia.com








