Oncolytic Virotherapy – An Overview
By Rajaneesh K. Gopinath, Ph.D.
In combination with cancer immunotherapy, this emerging field promises immense therapeutic value. Here’s an analysis of current trends.
The Concept
The idea of treating cancers with viruses is, surprisingly more than half a century old. As far back as 1912, an Italian clinician N. DePace observed that cervical cancer patients briefly displayed tumor regression post rabies vaccination (1). Soon after, Levaditi and Nicolau demonstrated viral oncolysis in the laboratory using mice. In 1949, it was discovered that the condition of several patients suffering from Hodgkin’s disease was ameliorated following treatment with hepatitis virus (2).
The traditional methods of cancer treatment such as chemotherapy have many downsides such as relapse, lack of specificity and cytotoxic side effects. In contrast, oncolytic virotherapy is relatively target-specific. This concept gained much traction only in the last 20 years, coinciding with the advent of genetic engineering. Over the years, several strategies have been implemented to minimize normal cell death without obstructing the efficacy of oncolysis. For instance, Reolysin, a naturally occurring variant of reovirus, is chosen because of its mild virulence in normal cells despite high oncolytic properties. Another example is Cavatak, the wild-type Coxsackievirus A21 which is under clinical trials. The more successful method employed in recent years is engineering recombinant viruses. In 1991, Herpes simplex virus type 1 (HSV1) became the first oncolytic virus to be genetically engineered (3).
The Underlying Molecular Mechanism
Tumor selectivity could largely be achieved by using recombinant viruses in cells that are overexpressing tumor-specific or viral entry specific receptors. As opposed to normal cells, the uncontrollable cell growth and impaired antiviral type I interferon signaling properties of cancer cells make them perfect hosts for elevated replication of viral particles. In summary, oncolytic virotherapy kills cancer cells in the following ways (4):
- Destroys tumor cells with impaired signaling
- Detects and kills tumor cells using engineered mutations or foreign genes
- By inducing antitumor immunity
- By expressing cytotoxic proteins
Successful Clinical Trials
A significant milestone arrived in 2015 when the US FDA approved the first oncolytic virus therapy, talimogene laherparepvec (T-VEC) developed by Amgen for treating metastatic melanoma (5). Prepared from a genetically engineered strain of herpes simplex virus 1 (HSV-1), it is deleted for two proteins ICP34.5 and ICP47 that normally performs the immune evasion function. As a result, the strain cannot kill normal cells but propagates in tumor cells where stress responses are already weakened. Some of the general considerations involved in the development of oncolytic viruses are safety, dosage, host resistance, toxicity, and adverse effects. In recent years a number of trials also take viral pharmacokinetics and pharmacodynamics into account.
In recent years many viruses such as Adenovirus, Vaccinia, Measles, and Polioviruses among others are being developed for cancer therapy. A search in 2016 alone reported around 40 ongoing clinical trials using oncolytic virotherapy (6).
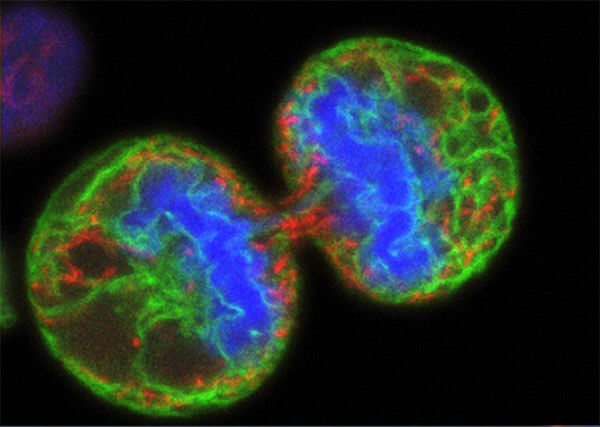
Credit: National Cancer Institute at NIH; Wellcome Images
Recent Innovations
In recent times, it is recognized that the success of oncolytic virotherapy could be enhanced by incorporating immune-stimulatory transgenes. In line with the developments in the cancer immunotherapy field, a number of clinical trials have combined oncolytic viruses with immune checkpoint inhibitors. Inhibitors such as pembrolizumab (anti-PD1) and ipilimumab (anti-CTLA4) are currently being tested in combination with T-VEC, Cavatak, and Reolysin (6).
In addition to this, many differentially expressed microRNAs and small molecule inhibitors are also tested in combination therapies. For instance, the adenovirus Ad5PTD (CgA-E1AmiR122) uses miR-122 to selectively replicate in and kill neuroendocrine cells (7). In a recent report, Zhang et al. performed a high throughput drug screen to identify synergistic compounds that could be combined with M1 oncolytic virus to treat hepatocellular carcinoma (8). Eeyarestatin I (EerI), an inhibitor of the valosin-containing protein (VCP) was identified from the screen to be the strongest sensitizer that increased the viral potency up to 3600-fold. Using several mouse models and hepatocellular carcinoma tissues, the authors found this combination suppressed the inositol-requiring enzyme 1α (IRE1α)–X-box binding protein 1 (XBP1) pathway triggering ER stress, eventually leading to apoptosis. They also demonstrated the tolerance of this therapeutic strategy in nonhuman primates.
In conclusion, the oncolytic virotherapy field is an exciting prospect to look forward to. One of the many challenges for the future is to determine the best combinatorial therapies for cancer treatment.
References
- https://www.ncbi.nlm.nih.gov/pubmed/13833074
- https://www.ncbi.nlm.nih.gov/pubmed/18134519
- https://www.ncbi.nlm.nih.gov/pubmed/1851332
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4923634/
- https://www.cancer.org/latest-news/fda-approves-imlygic-talimogene-laherparepvec-for-melanoma.html
- https://www.ncbi.nlm.nih.gov/pubmed/27441411
- https://www.ncbi.nlm.nih.gov/pubmed/21490682
- https://www.ncbi.nlm.nih.gov/pubmed/28835517
©www.geneonline.com All rights reserved. Collaborate with us: service@geneonlineasia.com









